How to Help Prevent Athlete’s Foot
 Getting a case of athlete’s foot can be annoying, for several reasons. First of all it causes itching between the toes, as the skin becomes dry and scaly. Second, in more severe cases, it can form blisters, cracks, and inflammation. Lastly, it spreads very easily, so try to avoid touching the affected area. Athlete’s foot is caused by a virus that thrives in moisture and dampness and is especially virulent in warmer temperatures. It is often picked up in swimming pools, locker rooms, and gyms, and it can be spread within the home in the shower or tub. It’s a good idea to wear protective foot coverings in damp or moist areas, keep your feet clean and dried – especially between the toes – as much as possible, and change your socks often if your feet have a tendency to become sweaty. There are several antifungal sprays and creams available over the counter that may bring some relief. If the condition persists, it may be a good idea to consult a podiatrist who can evaluate its severity and offer appropriate treatment options for you.
Getting a case of athlete’s foot can be annoying, for several reasons. First of all it causes itching between the toes, as the skin becomes dry and scaly. Second, in more severe cases, it can form blisters, cracks, and inflammation. Lastly, it spreads very easily, so try to avoid touching the affected area. Athlete’s foot is caused by a virus that thrives in moisture and dampness and is especially virulent in warmer temperatures. It is often picked up in swimming pools, locker rooms, and gyms, and it can be spread within the home in the shower or tub. It’s a good idea to wear protective foot coverings in damp or moist areas, keep your feet clean and dried – especially between the toes – as much as possible, and change your socks often if your feet have a tendency to become sweaty. There are several antifungal sprays and creams available over the counter that may bring some relief. If the condition persists, it may be a good idea to consult a podiatrist who can evaluate its severity and offer appropriate treatment options for you.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact one of our doctors from Coral Desert Foot & Ankle. Our doctors will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
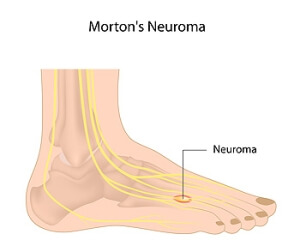
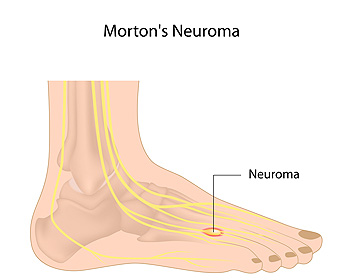
An Overview of Morton’s Neuroma
One common cause of foot pain is Morton’s neuroma, a thickening of the nerve tissue between the toes. This condition usually affects the space between the third and fourth toes and causes symptoms such as burning pain, tingling, numbness, and a strange sensation akin to walking on a pebble. Pain is often worsened by wearing shoes that are too tight or have high heels. Morton’s neuroma is diagnosed through medical history and physical examination. In some cases, imaging studies may be needed to rule out other causes of foot pain. Treatment is typically conservative and includes resting and icing the foot, wearing orthotics, and taking medications to reduce pain. If you have symptoms of Morton’s neuroma, please seek the care of a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our doctors of Coral Desert Foot & Ankle. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
How MLS Laser Therapy Sheds Light on Pain and Inflammation
MLS (Multiwave Locked System) Laser Therapy is a non-invasive method of treatment that uses two continuous therapeutic wavelengths of light that penetrate deep into the tissue to stimulate the regeneration of cells, decrease pain and inflammation, and improve circulation to the injured area. While there may be a slight warming sensation at the site of treatment, the combination of these two synchronized wavelengths minimizes the risk of thermal damage. Treatments generally take 10-15 minutes, and the typical course of treatment entails roughly 6 to 12 treatments. Many patients experience long-term positive results from MLS Therapy, as it addresses the cause of pain rather than simply masking symptoms. Podiatrists may use MLS therapy to treat plantar fasciitis, Achilles tendon issues, bursitis, neuromas, arthritis, fractures, injuries, and more. If you have any of these conditions, talk to your podiatrist to see if you are a good candidate for MLS Laser Therapy.
MLS Laser Therapy is a successful alternative for treating any pain you may be experiencing related to certain podiatric conditions. If you are interested in MLS Laser Therapy, consult with one of our doctors from Coral Desert Foot & Ankle. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
MLS Laser Therapy
Multiwave Locked System (MLS) Laser Therapy is a patented, FDA-cleared technology that helps relieve pain and inflammation from a number of podiatric conditions, including:
- Heel Pain
- Plantar Fasciitis
- Sports Injuries
- Wounds
- Achilles Tendonitis
- Arthritis
- Neuropathy
- Neuromas
MLS Laser Therapy is an ideal alternative to surgery and prescription medication, as it has no negative side effects and encourages accelerated healing. Among its many clinical benefits, MLS Laser Therapy also:
- Reduces swelling due to bruising or inflammation
- Blocks pain
- Reduces formation of scar tissue
- Improves nerve function
If you have any questions, please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
MLS Laser Therapy
MLS Laser Therapy is an FDA-approved technology designed to treat various painful conditions. It is often sought out as a successful alternative to surgical treatment and prescription medication that may otherwise bring about negative side effects. During MLS Laser Therapy, light energy enters the damaged cells to stimulate intercellular activity, reducing pain in the affected area and accelerating the recovery process.
MLS Laser Therapy is used in podiatry to treat various conditions. These include heel pain, plantar fasciitis, sports injuries, wounds, Achilles tendonitis, arthritis, neuromas, neurological pain, musculoskeletal disorders, and sore muscles. Aside from the specific conditions MLS Laser Therapy treats, patients can also gain from the treatment’s general benefits. These benefits include a rapid relief of pain, the reduction of swelling caused by inflammation or bruising, faster healing, improved blood circulation, the reduction of scar tissue, and improved nerve function.
MLS Laser Therapy is a non-surgical treatment with no side effects. The treatment process is painless and typically takes a short amount of time to complete. Several treatments may be required depending on the specific condition.
Am I at Risk of Developing Fungal Toenails?
Fungi that reside on the body can become overgrown over time in, or on, the toenail. This can result in an infection known as onychomycosis. You can also pick up the infection through contact with someone who has it. Further, this fungal infection can be transmitted through contact with toenail clippers, nail files or pedicure instruments at a salon where fungi are present. Older adults — whose drier nails make it easier for fungi to enter the nail — are more prone to developing fungal infections, as well as those who wear fake nails, use public swimming/showering areas, have diabetes, poor circulation, a nail injury, or a weakened immune system. People whose feet are confined to warm, moist environments where fungi thrive (i.e., dark boots or sneakers) are also more at risk of developing fungal nails. Fungal nail symptoms include brittle, thickened, discolored or distorted nails, which can sometimes be accompanied by odor or pain. While some people try to treat fungal toenail infections at home, the fungi are very stubborn and resilient. Professional treatment from a podiatrist is often necessary to quickly and completely eradicate the infection, and prevent it from recurring.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact one of our doctors of Coral Desert Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.