Causes of Seed Corns

Seed corns, those tiny yet painful annoyances on the feet, may sound inconsequential but can be quite uncomfortable. These small, hardened, and sometimes translucent bumps typically develop on the soles of the feet or in between the toes. They are a form of callus, but unlike the regular calluses that form due to friction or pressure, seed corns have a different origin. The causes of seed corns can vary. They often arise from dry skin, which is more prone to developing these small, central core calluses. Ill-fitting shoes that constantly rub against certain areas of the feet can also be a culprit. Additionally, foot deformities or gait abnormalities can increase pressure on specific spots, leading to seed corn formation. While seed corns may seem minor, they can be quite painful while walking. If you are dealing with these tiny irritations on your feet, it is suggested that you consult a podiatrist who can alleviate the discomfort and prevent them from returning, ensuring your feet remain healthy and pain-free.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact one of our doctors of Coral Desert Foot & Ankle. Our doctors will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Understanding Corns and Calluses
Corns and Calluses are both hardened layers of thickened skin that develop because of friction. Both ailments are typically found on the feet and may be unsightly. Although they have similarities, corns and calluses are different from each other.
Some causes of corns and calluses may be wearing ill-fitting shoes and not wearing socks. If you wear tight shoes, your feet will constantly be forced to rub against the shoes, causing friction. If you fail to wear socks, you are also causing your feet to endure excess friction.
There are some signs that may help you determine whether you have one of these two conditions. The first symptom is a thick, rough area of skin. Another common symptom is a hardened, raised bump on the foot. You may also experience tenderness or pain under the skin in addition to flaky, dry, or waxy skin.
There are also risk factors that may make someone more prone to developing corns and calluses. If you are already dealing with bunions or hammertoe, you may be more vulnerable to having corns and calluses as well. Other risk factors are foot deformities such as bone spurs, which can cause constant rubbing inside the shoe.
Corns tend to be smaller than calluses and they usually have a hard center surrounded by inflamed skin. They also tend to develop on the parts of the body that don’t bear as much weight such as the tops and sides of toes. Corns may also be painful for those who have them. On the other hand, calluses are rarely painful. These tend to develop on the bottom of the feet and may vary in size and shape.
Fortunately, most people only need treatment for corns and calluses if they are experiencing discomfort. At home treatments for corns and calluses should be avoided, because they will likely lead to infection. If you have either of these ailments it is advised that you consult with your podiatrist to determine the best treatment option for you.
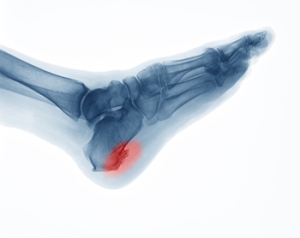
Definition and Root Causes of Heel Spurs
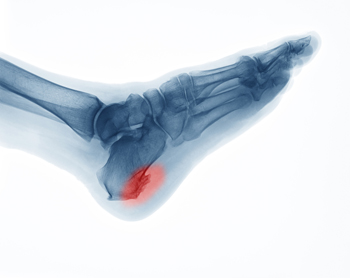
Heel spurs are bony growths that form on the underside of the heel bone or the back of the heel where the Achilles tendon attaches. These spurs are not sharp, unlike their name suggests, but they can cause excruciating discomfort by irritating the surrounding tissues. They often develop as a response to long-term strain on the foot's ligaments and muscles. Repetitive activities, such as running or standing for extended periods, improper footwear, and being overweight can contribute to the formation of heel spurs. Additionally, individuals with flat feet or high arches are more susceptible. While heel spurs may not always cause pain, when they do, it's typically due to inflammation of the nearby soft tissues. Understanding the definition and underlying causes of heel spurs empowers individuals to make informed choices in managing and preventing this sometimes debilitating foot condition. If you have heel pain, it is strongly suggested that you consult a podiatrist who can effectively diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our doctors from Coral Desert Foot & Ankle. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
The Harmony of Ankle Bones

Beneath the surface of our feet lies a delicate orchestra of bones, working seamlessly to provide stability and flexibility. The ankle bones are the unsung heroes of this intricate composition. These bones, namely the tibia, fibula, and talus, form a complex network that allows us to walk, run, and jump with precision. The tibia, the weight-bearing bone, supports our body's weight, while the fibula adds extra support and stability. The talus, perched atop the heel bone, serves as a vital link between the leg and the foot, enabling pivotal movements. These bones are finely tuned instruments, ensuring smooth walking and running on various terrains. Understanding how the bones in the ankles work together sheds light on the remarkable mechanics that keep us moving effortlessly. If you would like additional information about the various functions of the ankle bones, it is suggested that you speak with a podiatrist.
If you have any concerns about your feet, contact one of our doctors from Coral Desert Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The Importance of Biomechanics in Podiatry
Biomechanics and its related study deal with the forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
Biomechanics and its related study deal with forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
The history of studying biomechanics dates back to ancient Egypt at around 3000 B.C., where evidence of professional foot care has been recorded. Throughout the centuries, advances in technology, science, and an understanding of the human body led to more accurate diagnosis of conditions such as corns for example. In 1974, biomechanics garnered a large audience when Merton Root founded Root Lab to make custom orthotics. He proposed that corrections of certain conditions could be implemented to gain strength and coordination in the area. Due to his research, we still use his basic principle of foot orthotics to this day.
As technology has improved, so have the therapeutic processes that allow us to correct deficiencies in our natural biomechanics. Computers can now provide accurate readings of the forces, movements, and patterns of the foot and lower leg. Critical treatment options can be provided to patients now who suffer from problems that cause their biomechanics to not function naturally. The best results are now possible thanks to 3D modeling and computing technologies that can take readings and also map out what treatment will do to the affected areas.
These advanced corrective methods were able to come to light thanks to an increase in both the technologies surrounding biomechanics and also the knowledge of how they work naturally. For example, shoe orthotics are able to treat walking inabilities by realigning the posture deviations in patients caused by hip or back problems. Understanding foot biomechanics can help improve movement and eliminate pain, stopping further stress to the foot. Speak with your podiatrist if you have any of these problems.
Are Bunions Affecting Your Everyday Life?
Effective Stretches for the Achilles Tendon
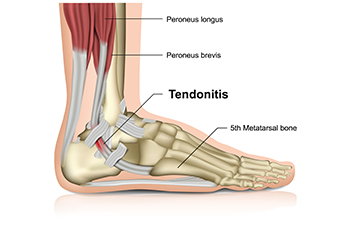
The Achilles tendon, located at the back of the ankle, plays a crucial role in walking, running, and jumping. To keep this vital tendon flexible and healthy, incorporating regular stretches into your routine is essential. One effective stretch is the calf stretch, which is done by standing while facing a wall, stepping one foot back, and leaning forward. The back leg remains straight with the heel on the ground. Another beneficial stretch is the seated calf stretch. This is accomplished by sitting with the legs extended, looping a towel around the ball of your foot, and gently pulling your toes towards you. Additionally, the downward dog yoga pose is fantastic for stretching the Achilles tendon. Remember to perform these stretches gradually and hold for approximately 20 to 30 seconds to enhance flexibility in addition to reducing the risk of developing an Achilles tendon injury. If you would like to learn more about stretches for the Achilles tendon, it is suggested that you make an appointment with a podiatrist for additional conversation.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our doctors of Coral Desert Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Causes and Treatment of Plantar Fasciitis

Plantar fasciitis is the most common cause of heel pain. Its main symptom is inflammation of the plantar fascia, the tissue connecting the front of the foot to the heel. Plantar fasciitis affects approximately 2 million patients each year, with athletes and individuals between 40 to 60 years of age being the most susceptible. The heel pain can range from sharp to dull, often worsening after prolonged periods of standing or physical activity. Causes of plantar fasciitis include repetitive physical activity, foot arch issues, and increased body weight. If left untreated, heel pain can lead to difficulty in walking. Fortunately, plantar fasciitis can be treated with proper care. Stretching exercises can help to rehabilitate the plantar fascia, and wearing proper footwear with adequate arch support is crucial. In some cases, wearing a foot brace or night splint can help to reduce swelling and alleviate pain. A podiatrist may suggest steroid shots or injections, as well as other pain relief medication, and in extreme cases, surgery may be considered. For help with problems associated with plantar fasciitis, it is suggested that you make an appointment with a podiatrist for an exam and treatment options.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our doctors from Coral Desert Foot & Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in St. George and Kanab, UT, and Mesquite, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.